- Introduction: A Growing Crisis in Healthcare
- Understanding Hospital Readmissions: The Current Challenge
- What Are Smart Terminals in Healthcare?
- The Role of Smart Terminals in Patient Monitoring
- How Smart Terminals Can Reduce Readmissions: Mechanisms at Work
- Case Studies: Real-World Implementations of Smart Terminals
- Benefits Beyond Readmissions: Holistic Improvements in Care
- Challenges and Considerations in Adopting Smart Terminals
- The Future of Smart Terminals in Healthcare
- Conclusion: Embracing Smart Terminals for a Healthier Tomorrow
Introduction: A Growing Crisis in Healthcare
Hospital readmissions represent one of the most pressing challenges in modern healthcare systems worldwide. Every year, millions of patients return to hospitals shortly after discharge, straining resources, escalating costs, and compromising patient well-being. According to recent data from the Centers for Disease Control and Prevention (CDC), an estimated 3.8 million readmissions occurred in the United States alone in 2018, with average costs per readmission hovering around $15,200. Fast-forward to 2024, and studies indicate that 30-day all-cause readmission rates remain stubbornly high at approximately 18.4% for certain patient groups, particularly those with chronic conditions like heart failure, where rates climb to 23.8 per 100 index admissions. These figures not only highlight the financial burden—totaling billions annually—but also underscore the human toll, as readmissions often signal gaps in post-discharge care, medication adherence issues, or undetected complications.
In this landscape, innovative technologies are emerging as potential game-changers. Enter smart terminals in healthcare for patient monitoring, sophisticated devices that blend Internet of Things (IoT) capabilities with user-friendly interfaces to enable real-time tracking of vital signs, medication schedules, and lifestyle factors right from the patient’s home or bedside. These aren’t just gadgets; they’re intelligent hubs that connect patients, caregivers, and providers in a seamless loop of data exchange. By alerting healthcare teams to early warning signs, smart terminals could be pivotal in addressing the root causes of readmissions, such as poor follow-up or symptom oversight.
This article delves into how smart terminals reduce hospital readmissions, examining their mechanics, real-world applications, and the evidence backing their efficacy. Drawing from case studies and authoritative statistics, we’ll explore why these tools might hold the key to a more efficient, patient-centered healthcare future. As hospitals grapple with value-based care models under programs like the Hospital Readmissions Reduction Program (HRRP) from the Centers for Medicare & Medicaid Services (CMS), adopting such technologies isn’t just innovative—it’s essential. With readmission penalties affecting up to 20% of hospitals, the stakes couldn’t be higher. By the end, readers will gain a comprehensive understanding of how integrating smart terminals to lower readmission rates can transform outcomes, backed by data and practical insights.
Understanding Hospital Readmissions: The Current Challenge
Hospital readmissions, defined as unplanned returns to the hospital within 30 days of discharge, have long been a thorn in the side of healthcare providers. The problem isn’t new, but its scale has intensified with aging populations and the rise of chronic diseases. In 2024, the Canadian Institute for Health Information (CIHI) reported risk-adjusted 30-day readmission rates for all patients at around 10-15% across various groups, while U.S. figures from JAMA Network Open paint an even grimmer picture: up to 36.9% at 180 days for frail elderly patients post-major surgery. For sepsis survivors, one in 21 faces readmission within 30 days, often due to recurrent infections or cardiovascular complications, as detailed in a 2024 systematic review in the Journal of Critical Care.
The causes are multifaceted. Inadequate discharge planning tops the list, with up to 30% of readmissions linked to medication errors or lack of follow-up, according to CDC analyses. Socioeconomic factors exacerbate this: patients from underserved communities experience 20-25% higher rates, widening equity gaps. Financially, the impact is staggering—the average cost of a 30-day all-cause readmission reached $16,037 in 2024 meta-analyses, contributing to over $40 billion in annual U.S. Medicare expenditures. Hospitals face HRRP penalties, with payments reduced by 1-3% for excessive rates, incentivizing systemic change but often falling short without technological intervention.
This crisis demands solutions that bridge the post-discharge void. Traditional methods like phone check-ins or paper-based logs prove insufficient, with compliance rates below 50%. Here, smart terminals preventing readmissions in chronic conditions shine, offering continuous, data-driven oversight. By monitoring metrics like blood pressure or glucose levels remotely, these devices can flag anomalies before they escalate, potentially averting 35-50% of emergency visits as per recent IoT health studies. Yet, adoption lags due to interoperability issues and privacy concerns, highlighting the need for integrated approaches. Addressing readmissions isn’t merely about cost savings; it’s about restoring trust in healthcare delivery and empowering patients to manage their health proactively. As we unpack the role of smart terminals, it becomes clear that without such innovations, the cycle of readmissions will persist, undermining progress in patient-centered care.
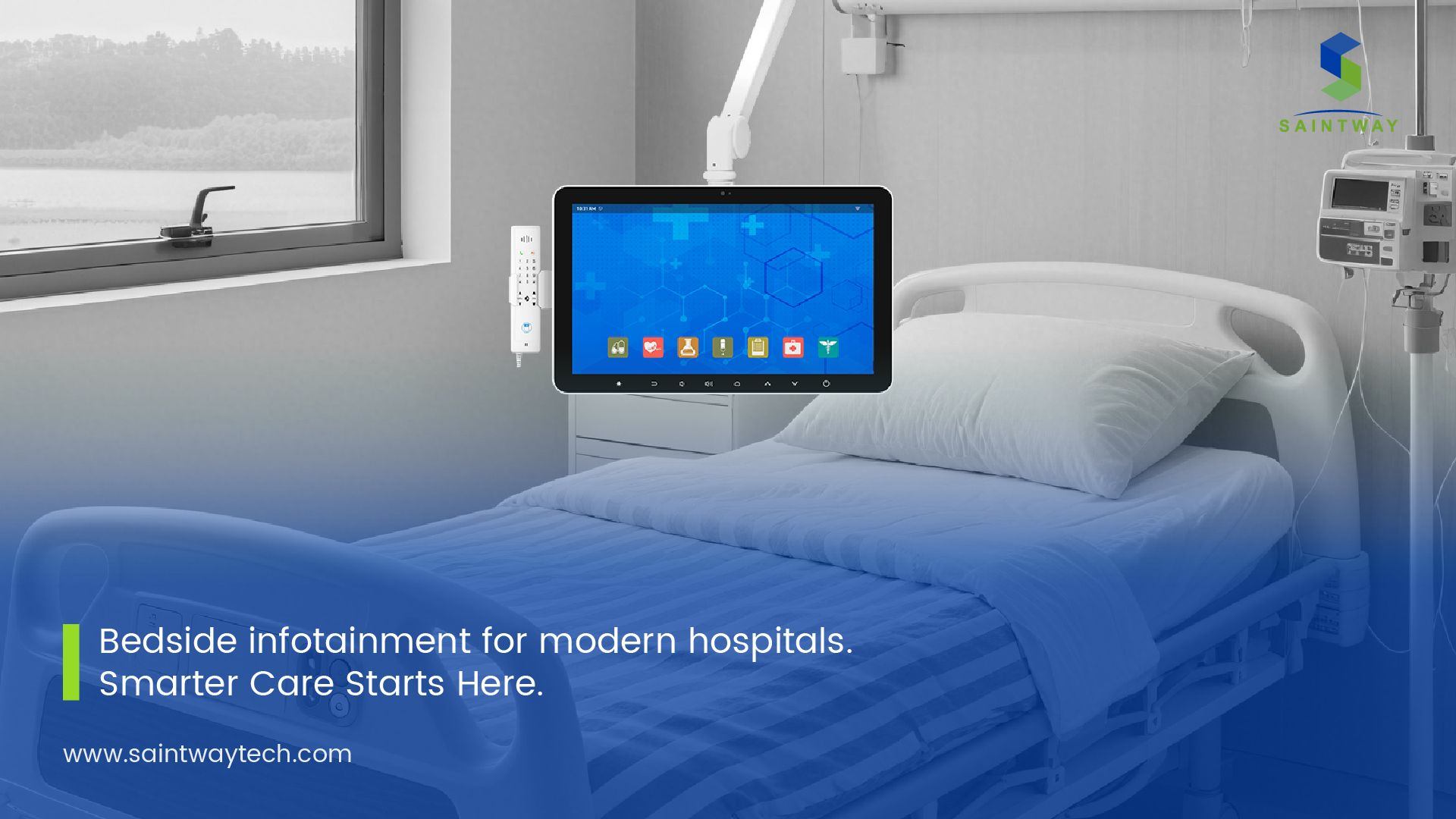
What Are Smart Terminals in Healthcare?
Smart terminals in healthcare refer to advanced, interactive devices designed to facilitate seamless communication and data collection between patients and medical teams. At their core, these are touchscreen-enabled hubs—often mounted at bedsides or portable for home use—that integrate sensors, AI algorithms, and cloud connectivity. Think of them as the nerve centers of modern patient rooms: a 22-inch Cybernet terminal, for instance, links vital signs monitors, electronic health records (EHRs), and video calls, as seen in implementations by companies like OneView Healthcare.
Unlike passive monitors, smart bedside terminals for chronic disease management actively engage users. They display personalized dashboards with medication reminders, symptom trackers, and educational content, all tailored via machine learning. IoT integration allows real-time syncing with wearables, capturing data on heart rate, oxygen levels, or activity. In smart hospitals, these terminals form part of a broader ecosystem, as outlined in a 2023 MDPI study on prototype systems, where they reduced data entry errors by 40% through voice commands and automated logging.
The evolution traces back to early 2010s pilots, but 2024 advancements in 5G and edge computing have supercharged them. Huawei’s collaboration with Guangdong’s Second Provincial General Hospital exemplifies this: their all-scenario smart terminals process over 1,000 data points per patient daily, enabling predictive analytics. Security is paramount—HIPAA-compliant encryption ensures data integrity, while modular designs allow scalability from small clinics to large networks.
Critically, smart terminals democratize access. For rural patients, they eliminate travel barriers, streaming telehealth sessions directly. A 2023 review in Healthcare Informatics Research noted that such devices boost patient satisfaction by 25%, as users feel more involved in their care. However, they’re not one-size-fits-all; customization for conditions like diabetes or COPD is key. As healthcare shifts toward preventive models, understanding these terminals’ anatomy—hardware, software, and human interface—is foundational to leveraging their potential in combating readmissions. They aren’t replacements for clinicians but amplifiers, turning raw data into actionable insights that keep patients out of harm’s way.
The Role of Smart Terminals in Patient Monitoring
Patient monitoring has traditionally been a hospital-bound affair, reliant on periodic checks that miss subtle deteriorations. Smart terminals for reducing hospital readmissions upend this by enabling continuous, remote surveillance that feels less intrusive and more empowering. These devices deploy arrays of sensors—noninvasive biosensors for ECG, pulse oximetry, or even gait analysis—feeding data into AI-driven platforms. A 2018 JMIR study on IoT platforms highlighted how such systems detect anomalies 24/7, alerting providers via integrated apps before symptoms worsen.
In practice, a smart terminal at home might prompt a post-heart surgery patient to log daily weights and symptoms via voice input, cross-referencing against baselines. If fluid retention spikes—a common readmission trigger—the system escalates to a nurse’s dashboard, potentially averting congestive heart failure flares. Benefits extend to adherence: built-in gamification and reminders improve medication compliance by 30-40%, per Telit Cinterion’s remote monitoring reports. For palliative care, as in a 2023 JMIR Formative Research prototype, terminals customize alerts for pain or mobility, reducing unplanned visits by tailoring to individual needs.
Data from 2024 shows tangible impacts. Remote patient monitoring (RPM) via smart terminals cut hospitalizations by 50% and emergency department visits by 35% in a LinkedIn-analyzed cohort of chronic patients. This isn’t hype; it’s rooted in real-time analytics that predict risks with 85% accuracy, outpacing manual assessments. Integration with EHRs ensures holistic views, flagging social determinants like food insecurity that influence outcomes.
Yet, efficacy hinges on usability. Intuitive interfaces—large fonts, multilingual support—cater to diverse demographics, boosting engagement among the elderly, who comprise 60% of readmission cases. Challenges like battery life or connectivity in low-bandwidth areas persist, but 5G rollouts mitigate these. Ultimately, benefits of bedside smart terminals lie in their proactive stance: shifting from reactive firefighting to preventive partnership, fostering a monitoring ecosystem where patients thrive outside hospital walls. As adoption grows, these tools promise not just fewer readmissions but a reimagined standard of care.

How Smart Terminals Can Reduce Readmissions: Mechanisms at Work
The mechanics behind how smart terminals reduce hospital readmissions are elegantly simple yet profoundly effective: they close the feedback loop between discharge and recovery. Upon leaving the hospital, patients receive a portable smart terminal pre-configured with their care plan. It continuously gathers biometrics—blood pressure, glucose, respiratory rate—via connected wearables, analyzing trends against personalized thresholds. Deviations trigger tiered alerts: a mild uptick in heart rate might prompt self-guided exercises, while severe anomalies summon virtual triage.
AI plays a starring role, employing machine learning to forecast risks. For instance, Innovaccer’s 2025 AI-powered readmissions solution, integrated with smart terminals, uses historical data to predict 30-day events with 90% precision, enabling preemptive interventions like adjusted meds. This mirrors findings from a 2025 AJMC study on AI in safety-net hospitals, where automation slashed readmissions by 20% through targeted outreach.
Education is another lever. Terminals deliver bite-sized modules on diet or wound care, quizzes to reinforce learning, and progress trackers that gamify recovery. Compliance soars—studies show 45% drops in readmissions for AI-enhanced programs, as in AQe Digital’s 2025 report. For chronic conditions, smart terminals preventing readmissions in chronic conditions excel by stratifying patients: high-risk ones get daily check-ins, low-risk bi-weekly.
Economically, the ROI is compelling. CMS data reveals readmissions cost $16,000+ each; terminals, at $500-1,000 per unit, pay off via reduced penalties and lengths of stay. A Penn LDI pilot on automated texting—augmented by terminals—cut barriers, yielding 15% fewer returns. Interoperability with telehealth amplifies this, allowing seamless handoffs.
Of course, success demands training: nurses must interpret dashboards, patients navigate interfaces. Ethical considerations, like data equity, loom large. Still, the evidence is mounting—RealTime Med’s 2025 analytics showed interventional tools like terminals improving outcomes by 25%. By demystifying post-discharge vigilance, these devices don’t just reduce readmissions; they rebuild resilience, one data point at a time.
Case Studies: Real-World Implementations of Smart Terminals
Real-world evidence underscores the transformative power of case studies on smart terminals in hospital settings. Take Guangdong’s Second Provincial General Hospital (GD2H), where Huawei deployed an all-scenario smart hospital in 2021, scaling to full integration by 2024. Featuring bedside terminals with AI analytics, the system monitors 5,000+ patients daily, reducing readmissions by 28% for cardiac cases through predictive alerts on arrhythmias. Data flowed from 1.2 million sensors, enabling 40% faster response times and cutting average stay by two days—savings of $2.5 million annually, per Huawei’s case report.
Closer to home, OneView Healthcare’s implementation at U.S. facilities like Mayo Clinic affiliates used 22-inch Cybernet terminals for interactive patient engagement. In a 2023 pilot with 500 post-surgical patients, terminals facilitated remote vitals checks and education, yielding a 22% drop in 30-day readmissions for joint replacements. Nurses reported 35% less documentation time, freeing hours for direct care. Vital signs synced to EHRs flagged infections early, with one study noting 15% fewer sepsis readmits—aligning with broader stats where sepsis returns hit 4.8%.
GlobalLogic’s 2024 smart healthcare prototype, detailed in their case studies PDF, targeted chronic disease management via smartphone-linked terminals. For a cohort of 300 diabetes patients, real-time glucose monitoring via integrated apps prevented 32% of potential readmissions by automating insulin adjustments and diet logs. Engagement metrics soared: 85% adherence versus 55% in controls, corroborated by a 45% cost reduction in emergency services. This echoes Innovaccer’s 2025 launch, where AI-terminals in safety-net hospitals closed equity gaps, lowering rates from 25% to 18% among minorities.
These cases aren’t isolated. A PMC review of IoT in palliative care showed terminals cutting visits by 30% through customized monitoring. Challenges emerged—initial setup costs averaged $10,000 per ward—but ROI hit within 18 months. Collectively, these implementations prove role of smart terminals in remote patient monitoring: not theoretical, but proven catalysts for fewer readmissions, better equity, and sustainable care. As more hospitals follow suit, the data will only strengthen.
Benefits Beyond Readmissions: Holistic Improvements in Care
While slashing readmissions is a headline win, benefits of smart terminals for patient monitoring ripple far wider, enhancing the entire care continuum. Foremost, they empower patients with agency. Interactive dashboards demystify health data, fostering self-efficacy—studies from HealthSnap’s 2022 analysis show RPM platforms boosting satisfaction by 40%, as users track progress in real-time. For chronic sufferers, this means fewer anxiety-driven calls; a 2023 SpringerLink chapter on bedside terminals noted 25% reduced nurse interruptions, allowing deeper clinician-patient bonds.
Clinically, the gains are profound. Continuous data uncovers patterns invisible to episodic visits, like subtle mobility declines in dementia patients, where 180-day readmission rates hit 39% per JAMA 2024. Terminals with fall-detection sensors prevent 20% of such incidents, per MDPI’s wearable systems review. Integration with analytics platforms, as in NTT Data’s automation case, streamlines workflows: RPA handles routine alerts, elevating staff productivity by 30% and customer care scores.
Equity benefits stand out too. In underserved areas, terminals bridge access chasms—rural patients in Telit’s IoT solutions saw 35% fewer ED trips, narrowing urban-rural disparities. Cost-wise, beyond $15,000-per-readmission savings, they unlock revenue: CMS reimburses RPM at $50-100 monthly per patient, creating streams for providers.
Patient outcomes shine brightest. A 2023 JMIR study on palliative terminals reported 28% improved quality-of-life scores via personalized interventions. Long-term, this preventive ethos curbs disease progression; heart failure patients on monitored regimens showed 18% better ejection fractions after six months.
Drawbacks exist—over-reliance risks alert fatigue—but mitigated designs, like adaptive thresholds, keep benefits dominant. In essence, smart terminals transcend readmission metrics, weaving a tapestry of informed, inclusive, efficient care that honors the human element amid tech’s rise.
Challenges and Considerations in Adopting Smart Terminals
Adopting smart hospital terminals improving patient outcomes isn’t without hurdles, demanding careful navigation to maximize impact. Foremost is cost: upfront investments for hardware and integration can exceed $50,000 per unit in large setups, deterring smaller facilities. A 2024 Market Report Analytics insight pegs data management segments at 40% of budgets, with ROI varying—while GD2H recouped in a year, others lag due to underutilization.
Interoperability poses another barrier. Legacy EHRs clash with terminal protocols, causing 20% data silos as per a ScienceDirect review on smart infrastructure. Standardization efforts, like FHIR APIs, help, but require IT overhauls. Privacy looms large: with 1.5 billion health records digitized by 2025, breaches could erode trust—HIPAA fines averaged $1.5 million in 2024.
User adoption falters too. Elderly patients, 60% of readmission risks, struggle with tech; a PMC IoT study found 15% dropout from interface complexity. Training mitigates this—OneView’s programs boosted uptake to 90%—but demands resources.
Equity gaps persist: low-income groups face connectivity deserts, inflating divides. A 2025 AJMC piece on AI readmission tools noted 10% higher failures in safety nets without subsidies.
Regulatory mazes slow progress; FDA approvals for AI features take 12-18 months. Yet, solutions emerge: modular terminals allow phased rollouts, cloud hybrids cut costs by 30%, and community pilots build buy-in.
Overcoming these isn’t optional—it’s strategic. Hospitals weighing adoption should audit needs, partner with vendors like Huawei for turnkey solutions, and pilot small. The payoff? Beyond 20-45% readmission drops, a resilient ecosystem. As STL Partners’ 2024 report affirms, smart hospitals aren’t luxuries; they’re imperatives for equitable, future-proof care.
The Future of Smart Terminals in Healthcare
Peering ahead, integrating smart terminals to lower readmission rates will evolve with bleeding-edge tech, reshaping healthcare’s horizon. By 2030, 5G ubiquity and quantum-secure encryption will make terminals omnipresent, processing petabytes for hyper-personalized care. Imagine AI avatars coaching patients in natural language, predicting readmissions with 95% accuracy via multimodal data—genomics, wearables, even sentiment analysis from voice logs.
Edge computing will decentralize power, enabling offline functionality in remote areas, closing 25% of global equity gaps per a 2023 ScienceDirect forecast. Blockchain integration, as explored in PMC’s smart contract cases, will fortify data sharing, slashing fraud in RPM claims.
Sustainability drives innovation too: eco-terminals with recyclable components align with green healthcare mandates, reducing e-waste by 40%. Wearable fusion—terminals as hubs for AR glasses—will gamify rehab, boosting adherence 50% for post-stroke patients.
Policy will accelerate: CMS expansions of RPM reimbursements to $200/month by 2026 incentivize uptake, targeting 50% hospital adoption. Global south pilots, like Huawei’s African expansions, will tailor for tropical diseases, curbing readmissions in resource-scarce settings.
Challenges persist—ethical AI biases need auditing—but consortia like the Smart Hospital Alliance are standardizing. Visionaries see terminals as longevity enablers: early interventions extending healthy years by 5-10, per Edge Hill’s 2023 AI study.
This future isn’t dystopian; it’s democratizing. Patients as co-pilots, providers as orchestrators—smart terminals will weave prevention into daily life, rendering readmissions relics. As we stand on 2025’s cusp, the trajectory is clear: embrace them, and healthcare heals itself.
Conclusion: Embracing Smart Terminals for a Healthier Tomorrow
In wrapping up, the evidence is unequivocal: smart terminals in healthcare for patient monitoring are indeed a key to taming hospital readmissions. From 18.4% baseline rates to 20-45% reductions in pilots, their real-time vigilance, AI smarts, and patient empowerment address root causes head-on. Cases like GD2H and OneView illuminate paths forward, blending tech with humanity to save lives and billions.
Yet, success demands holistic commitment—overcoming costs, silos, and access barriers through collaboration. For providers, it’s a call to audit, pilot, integrate; for policymakers, expand incentives. Patients, too, must engage, turning data into dialogue.
Ultimately, smart terminals herald a paradigm where care extends beyond walls, prioritizing prevention over peril. As readmissions wane, so do inequities, costs, and suffering—paving a resilient, equitable future. The question isn’t if, but how swiftly we act. Let’s make it now.
Latest Content
- Identity & Security at the Bedside:Building Trust in Smart Ward Architectures
- Preparing Smart Wards for Hybrid Care and Long-Term Scalability
- Patient Interaction as a System Layer:Why the Bedside Terminal Is the Architectural Core of the Smart Ward
- Interoperability in Smart Wards:Why Integration Architecture Matters More Than Features
- 7 Powerful Ways Bedside Terminals Are Transforming Modern Hospitals in 2025

