In smart wards, digital transformation is no longer limited to connecting devices or digitizing workflows. The true challenge lies deeper:
How can hospitals ensure that the right person accesses the right information, at the right moment, in the right context?
At the bedside—where clinical decisions, patient interactions, and sensitive data converge—identity and security are not technical details. They are foundational elements of trust.
As hospitals across Europe, North America, and other advanced healthcare markets expand smart ward deployments, identity and security are becoming architectural priorities rather than afterthoughts.

The Bedside as a Security Boundary
Traditionally, hospital identity management has focused on centralized systems:
HIS, EMR, identity directories, and access management platforms.
However, the bedside introduces a new layer of complexity.
At the point of care, multiple identities coexist:
· Clinicians accessing patient records
· Nurses performing workflow tasks
· Patients interacting with digital services
· Family members engaging with bedside interfaces
· Devices communicating with backend systems
Each interaction involves different permissions, risks, and expectations.
In smart wards, the bedside is no longer just a screen.
It is a security boundary where clinical systems, human identities, and digital interfaces intersect.
Why Traditional Identity Models Fall Short
Many hospitals still rely on identity models designed for desktop environments:
· Static login credentials
· Role-based access defined at system level
· Centralized authentication without contextual awareness
These approaches struggle in smart ward scenarios, where:
· Clinicians move rapidly between patients and locations
· Devices are shared across shifts
· Patients interact with systems without formal credentials
· Hardware lifecycles extend far beyond software updates
· Multiple vendors coexist within a single ward
The result is a gap between security policies and real-world workflows.
When identity systems are disconnected from bedside interactions, hospitals face:
· Over-permissioned access
· Workarounds that bypass security controls
· Fragmented audit trails
· Increased risk of data exposure
· Reduced clinician efficiency
Identity as a Contextual Layer, Not a Login Step
In modern smart ward architectures, identity must evolve from a simple authentication mechanism into a contextual layer.
This means identity should be dynamically shaped by:
· User role (clinician, nurse, patient, visitor)
· Location (ward, bed, department)
· Device type (bedside terminal, mobile device, workstation)
· Workflow state (consultation, medication, discharge)
· Time and operational context
At the bedside, identity is not static.
It is continuously negotiated between people, devices, and systems.
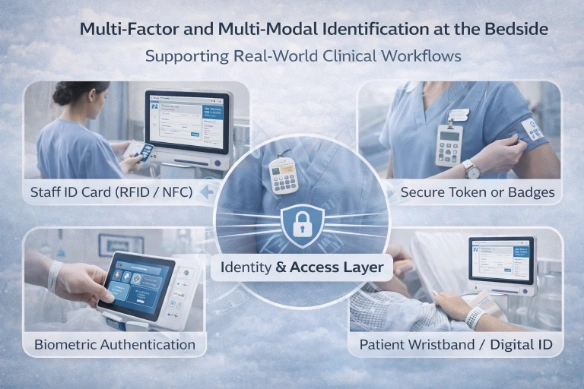
Multi-Factor and Multi-Modal Identification at the Bedside
To support real-world clinical workflows, smart wards increasingly adopt multi-modal identity mechanisms, such as:
· Staff ID cards (RFID / NFC)
· Secure tokens or badges
· Biometric authentication
· Context-aware session switching
· Patient identification via wristbands or digital IDs
These methods reduce reliance on passwords while aligning security with clinical efficiency.
More importantly, they enable identity to travel with the user—not remain locked to a workstation.
Security Beyond Users: Device Identity Matters
In smart wards, devices themselves are actors in the security model.
Every bedside terminal, mobile device, and IoT component must be treated as an identity-bearing entity.
This requires:
· Device authentication and certification
· Secure communication channels
· Policy-based device access control
· Lifecycle management across hardware deployments
· Integration with hospital identity frameworks
Without device-level identity, even the most robust user authentication systems remain vulnerable.
The Hidden Risk: Fragmented Identity Across Systems
One of the most underestimated risks in smart wards is identity fragmentation.
When each subsystem—EMR, nurse call, IPTV, patient engagement, RTLS—implements its own identity logic, hospitals face:
· Inconsistent access policies
· Redundant authentication processes
· Limited cross-system traceability
· Increased integration complexity
True interoperability is impossible without identity interoperability.
Designing Identity-First Smart Ward Architectures
Leading hospitals and system integrators are shifting toward identity-first architecture principles:
1. Unified Identity Layer
Identity services should span clinical systems, devices, and patient interfaces.
2. Loose Coupling Between Identity and Applications
Applications should consume identity services rather than implement their own.
3. Context-Aware Access Control
Permissions should adapt to clinical workflows and bedside contexts.
4. Continuous Authentication
Identity should be validated throughout interactions, not only at login.
5. Auditability by Design
Every bedside interaction should be traceable across systems.
These principles transform identity from a compliance requirement into an enabler of safe, scalable digital care.
Identity and Security as Experience Factors
In smart wards, security is often perceived as a trade-off against usability.
Yet the opposite is true.
When identity and security are designed correctly:
· Clinicians spend less time logging in and switching systems
· Patients feel safer interacting with digital services
· Integrators can deploy new applications with lower risk
· Hospitals gain confidence in scaling digital initiatives
Security, in this sense, becomes part of the patient and clinician experience.
Smart Wards Are Built on Trust
A smart ward is not defined by screens, devices, or features.
It is defined by trust—between people, systems, and technology.
At the bedside, identity and security are not peripheral concerns.
They are the invisible infrastructure that makes digital care possible.
In the long term, hospitals that treat identity as an architectural foundation—not a technical checkbox—will be best positioned to scale innovation without compromising safety.
Latest Content
- Preparing Smart Wards for Hybrid Care and Long-Term Scalability
- Patient Interaction as a System Layer:Why the Bedside Terminal Is the Architectural Core of the Smart Ward
- Designing Workflow-Centered Hospital Systems: Lessons from Real Ward Environments
- The Global Leaders Shaping Interaction: Top Touch Screen Manufacturers Driving Innovation
- Smart Ward Trends 2026: How Advanced Hospitals Are Redefining Digital Care

