For decades, hospital wards were designed around a simple assumption: care happens inside the hospital.
That assumption no longer holds.
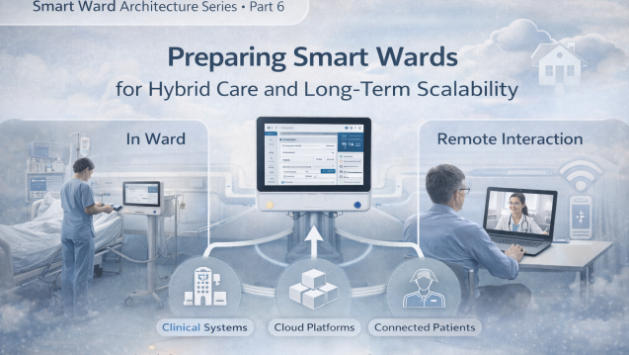
Remote monitoring, telemedicine, digital therapeutics, and home-based care are rapidly reshaping how healthcare is delivered. The smart ward is no longer a closed environment—it is becoming a hybrid ecosystem that connects bedside, cloud, clinicians, and patients beyond hospital walls.
In this context, scalability is no longer a technical option. It is a strategic requirement.
1) From Smart Wards to Hybrid Care Ecosystems
Traditional smart ward projects focused on digitizing in-ward workflows:
- Nurse call systems
- Bedside terminals
- IPTV and infotainment
- Clinical data integration
- Patient engagement interfaces
Today, hospitals are extending these capabilities beyond physical wards:
- Remote patient monitoring
- Virtual consultations
- AI-assisted clinical decision support
- Cross-facility data sharing
- Continuity of care after discharge
The smart ward is evolving into a node within a larger digital care network.
This shift fundamentally changes how smart ward architecture must be designed.
2) The Scalability Challenge: More Than Performance
When hospitals talk about scalability, they often think about hardware capacity or network bandwidth.
In reality, smart ward scalability has three dimensions:
Technical Scalability
Can systems handle growing data volumes, users, and devices without disruption?
Architectural Scalability
Can new applications, vendors, and workflows be added without redesigning the entire system?
Organizational Scalability
Can digital systems adapt to new care models, policies, and clinical practices?
Most smart ward failures happen not at the technical layer, but at the architectural and organizational layers.
3) Mixed Lifecycles: The Hidden Constraint
One of the most underestimated challenges in smart wards is lifecycle mismatch:
- Software evolves every 6–12 months
- Clinical workflows evolve continuously
- Hardware infrastructure remains deployed for 3–5 years or longer
- Regulatory requirements change unpredictably
If architecture is not designed for mixed lifecycles, innovation becomes expensive and risky.
In hybrid care environments, this challenge is amplified.
4) Bedside as a Hybrid Care Interface
In future-ready smart wards, the bedside is no longer just a display—it is a hybrid interaction layer.
At the bedside, multiple worlds intersect:
- Clinical systems (EMR, nurse call, workflows)
- Patient-facing digital experiences
- Remote care platforms
- Identity and access control
- Real-time communication
A scalable smart ward architecture treats the bedside as an integration point, not a standalone device.
This perspective changes how hospitals and integrators evaluate bedside solutions.
5) Designing for Long-Term Scalability
Hospitals that succeed in hybrid care environments share common design principles:
Platform-Oriented Architecture
Instead of building isolated solutions, they design platforms that support multiple applications and integrations.
API-First Integration
Systems expose standardized interfaces, enabling rapid integration of new services.
Modular Deployment
Components can be upgraded independently without disrupting the entire ward.
Vendor-Agnostic Strategy
Hospitals avoid dependence on a single technology stack, preserving flexibility.
Context-Aware Interaction
Systems adapt to user roles, clinical context, and care settings.
Scalability is not achieved through technology alone—it is achieved through design philosophy.
6) Why Hybrid Care Changes the Role of System Integrators
In the past, system integrators focused on connecting devices and software.
In hybrid smart wards, their role expands:
- Designing integration architecture
- Orchestrating multi-vendor ecosystems
- Aligning digital systems with clinical workflows
- Ensuring long-term adaptability
System integrators are becoming digital architects of healthcare environments.
7) Smart Wards Are No Longer Physical Spaces
A smart ward is no longer defined by walls, beds, or devices.
It is defined by connectivity, interoperability, and scalability.
Hospitals that prepare for hybrid care today are not just upgrading technology—they are redefining how care is delivered.
Closing Statement
The Bedside Is No Longer Just a Device. It Is Becoming the Core Interaction Layer of Smart Ward Architecture.
In the Smart Ward Architecture series, we explore how hospitals, software developers, and system integrators can design future-ready digital care environments—where bedside systems, clinical platforms, and hybrid care models work as one.
Latest Content
- Identity & Security at the Bedside:Building Trust in Smart Ward Architectures
- Patient Interaction as a System Layer:Why the Bedside Terminal Is the Architectural Core of the Smart Ward
- Designing Workflow-Centered Hospital Systems: Lessons from Real Ward Environments
- Smart Ward Trends 2026: How Advanced Hospitals Are Redefining Digital Care
- Interoperability in Smart Wards:Why Integration Architecture Matters More Than Features

