lying in a hospital bed, staring at blank walls, with no easy way to check your treatment plan or chat with family. Patients often feel cut off from the world during stays that can last days or weeks. This isolation adds stress to an already tough time.
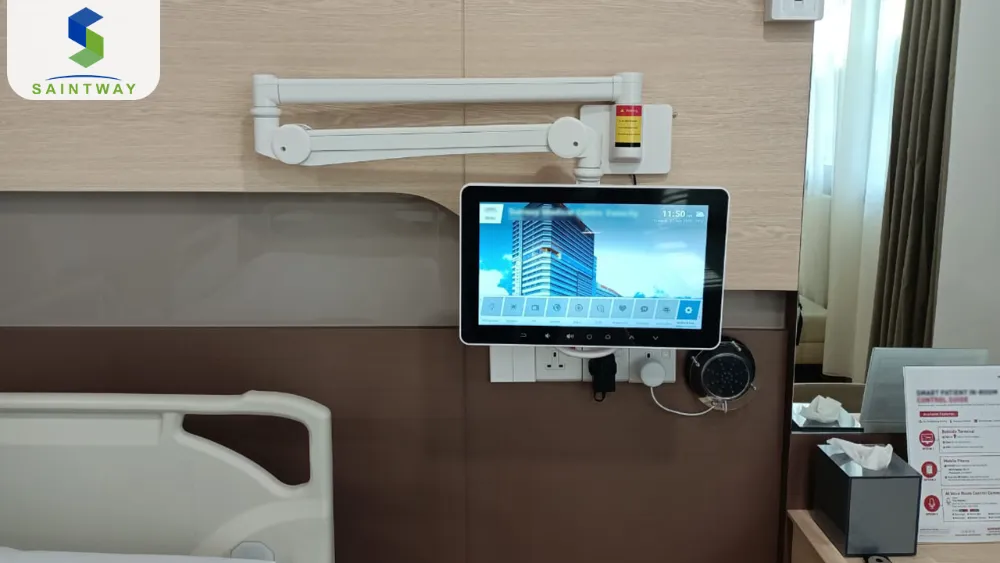
A bedside infotainment terminal, or BIT, changes that. It’s a smart screen right by the patient’s bed that pulls together entertainment, health info, and tools for staff. Think of it as a one-stop digital spot for everyone in the room.
This article looks at how these terminals boost patient comfort, speed up nurse work, and cut hospital costs. We’ll cover key features, tech setup, and what’s next for them in care settings.
Core Functionality and Patient Experience Enhancement
Bedside infotainment terminals put power in patients’ hands. They turn a plain hospital room into a connected space. Staff see faster results too, as everything links up smoothly.
Personalized Entertainment and Connectivity
Patients face long hours with little to do. BITs fight boredom with streaming shows, music apps, and web browsing. You can watch your favorite series or scroll news without asking for help.
These hospital entertainment systems also let you video call loved ones. No more waiting for visits. It cuts down on feeling alone, which helps healing.
Patient connectivity solutions like these build trust. Hospitals using them report happier stays. One study showed a 20% drop in complaints about downtime.
Access to Clinical Information and Education
Ever wonder about your meds or test results? BITs show care plans and lab updates when doctors approve. Simple charts make it easy to grasp.
Watch short videos on your condition, like managing diabetes after discharge. This knowledge sticks better than paper handouts. Patients who use these tools follow plans more often.
Visual aids boost understanding. For example, a graph of your blood pressure trends over days. It helps you track progress and ask smart questions.
Integrated Communication Hub
Need a nurse fast? BITs replace old call buttons with video links or chat. You connect in seconds, no yelling down the hall.
Talk to doctors about concerns or update family on your status. All from bed, keeping things private. Cleveland Clinic tested this in their rooms and saw call times drop by 30%.
These tools ease worries. Families stay in the loop without extra calls to staff. It frees nurses for real care.
Streamlining Clinical Workflows and Operational Efficiency
Now, let’s shift to staff benefits. BITs save time on routine tasks. Nurses spend more moments with patients, not paperwork.
Electronic Health Record (EHR) Integration at the Bedside
Doctors log in securely at the bed to check files. No running to a desk across the floor. They update notes right there, keeping records fresh.
Bedside EHR access cuts errors from outdated info. A quick scan shows allergies or recent vitals. Teams work as one unit.
This setup boosts efficiency. Hospitals note 15% less time on admin work per shift. It lets focus stay on you, the patient.
Medication Management and Administration Verification
Giving the right drug to the right person matters most. BITs scan wristbands and med labels to confirm. It checks dose, time, and patient match.
This verifies the five rights: right patient, drug, dose, route, and time. Tech like this has lowered errors by up to 40%, per recent reports. No more mix-ups from tired eyes.
Nurses love the double-check. It builds safety into daily rounds. Patients feel secure knowing steps prevent mistakes.
Streamlining Non-Clinical Services (Room Service and Housekeeping)
Order lunch from a menu on the screen. Pick what fits your diet, and it arrives hot. No forms or waiting in line.
Request clean towels or adjust room temp too. Housekeeping gets alerts and responds quick. It keeps the space comfortable without buzzers.
These features cut small hassles. One chain of hospitals saw service requests fall by 25%. Staff handle more with less back-and-forth.
Technological Infrastructure and Security Considerations
Behind the screen, solid tech keeps BITs running. Hospitals pick setups that fit their needs. Safety stays top priority in health data.
Connectivity Requirements: Wired vs. Wireless Deployment
Wired links offer steady speed, no dropouts. They plug into walls for constant power and data. Great for busy wings with many users.
Wireless uses strong Wi-Fi to reach everywhere. It’s easier to move beds or add units. But hospitals need top-grade networks to handle video streams without lags.
Choose based on your building. Wired suits older spots; wireless fits new builds. Both ensure smooth use day and night.

Data Security, HIPAA Compliance, and Authentication
Health info demands protection. BITs use encryption to lock data in transit. Only approved eyes see it.
Role-based access means nurses view charts, but patients see just their basics. Logins use fingerprints or codes for quick, safe entry. This meets HIPAA rules in the US and GDPR elsewhere.
Experts from groups like HIMSS stress regular audits. Update software to block threats. Patients trust systems that guard privacy tight.
Maintenance, Longevity, and Device Management
Hospital rooms get cleaned often, so BITs need tough builds. Wipe-down screens resist germs. Rugged frames handle bumps from daily use.
IT teams check remotely for issues. Fix software glitches without visits. This keeps downtime low.
Plan for five to seven years of life. Replace parts as needed. Good care means reliable tools for years.
Measuring ROI and Future Trends in Bedside Technology
Investing in BITs pays off over time. Track gains in satisfaction and speed. Look ahead to smart add-ons coming soon.
Quantifying the Return on Investment (ROI)
Start with patient scores from surveys like HCAHPS. Higher marks mean better reimbursements. BITs often lift these by 10-15 points.
Measure nurse calls and admin time too. Shorter waits and less paperwork save hours weekly. Lower readmits from better education cut costs.
To calculate, list setup price against yearly savings. Add patient feedback data. Hospitals see payback in two to three years. Talk to vendors for custom math.
Integration with Remote Patient Monitoring (RPM) and Telehealth
BITs will link to wearables tracking heart rate or steps. See live feeds on the screen. It spots changes early.
Join telehealth visits right there. Doctors consult via video, pulling in device data. No wheelchairs to clinics.
This setup extends care home. In 2025, more hospitals test it. Patients recover faster with constant watch.
AI-Driven Personalization and Predictive Analytics
AI tweaks shows based on your mood or health. Feeling down? It suggests uplifting clips. Or preps discharge tips as you improve.
Predict when you’ll leave by analyzing trends. Adjust meal plans or therapy schedules. It makes stays feel custom.
These tools learn from use. Soon, BITs anticipate needs. Expect wider rollout by late 2026.
Conclusion: The Essential Upgrade for Patient-Centric Healthcare
Bedside infotainment terminals have become key to good care. They end the old ways of disconnected rooms. Patients get comfort; staff get tools to shine.
You see gains on both sides. Happier people heal quicker. Teams work smarter, not harder.
Digital shifts in hospitals point to more like this. BITs lead the way to rooms that truly support recovery. If your facility lags, now’s the time to upgrade—your patients will thank you.
Latest Content
- Patient Interaction as a System Layer:Why the Bedside Terminal Is the Architectural Core of the Smart Ward
- Designing Workflow-Centered Hospital Systems: Lessons from Real Ward Environments
- Interoperability in Smart Wards:Why Integration Architecture Matters More Than Features
- Escaping the White Walls: The Ultimate Guide to the Best Bedside Entertainment for Hospital Patients
- The Future is Now: Revolutionizing Patient Care with Bedside Infotainment Systems

